Mohs Surgery Success Rates
Mohs surgery is recognized for its effectiveness in treating certain types of skin cancer. This page explains how success rates are measured, what factors influence outcomes, and why Mohs surgery is often chosen for high-risk or sensitive areas.
When facing a skin cancer diagnosis, many patients want to understand how effective a treatment is and what the medical evidence shows. Mohs surgery is widely recognized for its high success rates, based on decades of clinical use and long-term studies. By removing skin cancer layer by layer and examining each layer under a microscope during the procedure, Mohs surgery allows for precise cancer removal while preserving healthy skin.
Understanding Mohs Surgery Success Rates
Success rates for skin cancer treatment can be confusing, especially when different terms are used. Understanding how success is measured can help patients better interpret medical information and set realistic expectations about treatment outcomes.
What “Success Rate” Means in Skin Cancer Treatment
In skin cancer treatment, a “success rate” generally refers to how effectively a procedure removes the cancer and prevents it from returning in the treated area. These rates are based on large clinical studies that follow patients over time.
Success rates do not predict individual outcomes. They reflect overall results seen across many patients and depend on factors such as the type of skin cancer, whether it is a first-time or recurrent tumor, and how long patients are monitored after treatment.
Cure Rate vs. Recurrence Rate
The cure rate describes the percentage of patients whose skin cancer does not return after treatment within a defined follow-up period. Mohs surgery is known for high cure rates because the surgeon examines 100% of the surgical margins during the procedure.
The recurrence rate refers to how often skin cancer comes back at the same site after treatment. Lower recurrence rates indicate more complete cancer removal. While Mohs surgery has low recurrence rates compared to many other treatments, no procedure can guarantee that skin cancer will never return.
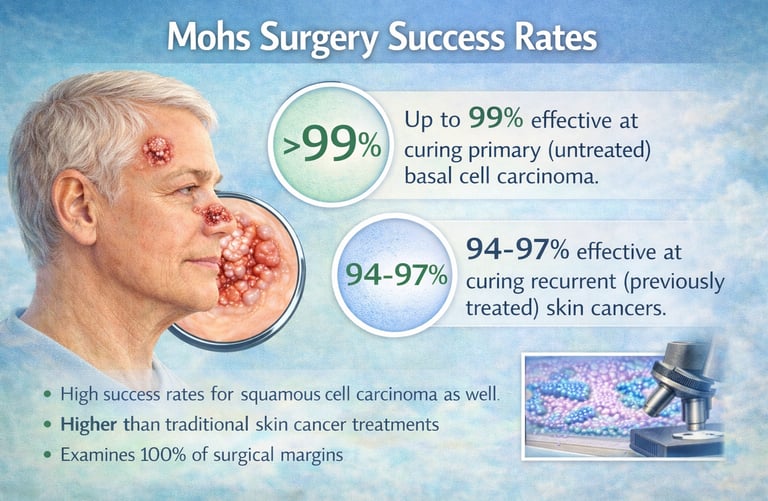
Overall Cure Rates for Mohs Surgery
Mohs surgery has been studied extensively and is recognized for its high cure rates in the treatment of certain skin cancers. These outcomes are based on long-term follow-up data and reflect the precision of examining all surgical margins during the procedure.
Primary Skin Cancers
Primary skin cancers are those being treated for the first time. For common skin cancers such as basal cell carcinoma and squamous cell carcinoma, Mohs surgery demonstrates very high cure rates when used appropriately.
Studies have shown that Mohs surgery achieves cure rates of up to 99% for primary basal cell carcinoma and approximately 97–98% for primary squamous cell carcinoma. These high rates are attributed to the thorough microscopic evaluation of tissue during surgery.
Recurrent Skin Cancers
Recurrent skin cancers are those that have returned after previous treatment. These tumors can be more challenging to treat because they may have irregular growth patterns or deeper extensions.
For recurrent basal cell carcinoma and squamous cell carcinoma, Mohs surgery continues to show strong results, with reported cure rates of approximately 94–96%. The ability to precisely track and remove remaining cancer cells makes Mohs surgery especially valuable for previously treated or complex tumors.
While these statistics are reassuring, individual outcomes vary, and long-term skin monitoring remains an important part of care.
Success Rates by Type of Skin Cancer
Mohs surgery is most commonly used to treat basal cell carcinoma and squamous cell carcinoma. Success rates vary slightly depending on the type of skin cancer, whether it is new or recurrent, and specific tumor characteristics.
Basal Cell Carcinoma
Basal cell carcinoma is the most common type of skin cancer and is often very responsive to Mohs surgery. When treated with Mohs surgery, basal cell carcinoma has some of the highest reported cure rates in dermatologic surgery.
For primary basal cell carcinoma, cure rates are reported to be up to 99%. For recurrent basal cell carcinoma, cure rates are typically around 94–96%. Mohs surgery is especially helpful for basal cell cancers located on the face or those with poorly defined borders.
Squamous Cell Carcinoma
Squamous cell carcinoma can be more aggressive than basal cell carcinoma, particularly in certain locations or in patients with weakened immune systems. Mohs surgery is often recommended for higher-risk squamous cell carcinomas.
Reported cure rates for primary squamous cell carcinoma treated with Mohs surgery are approximately 97–98%, while recurrent squamous cell carcinoma has cure rates of about 94–95%. Careful removal and ongoing follow-up are important, as squamous cell carcinoma has a higher risk of recurrence than basal cell carcinoma.
Even with high success rates, regular skin exams remain essential after treatment.
Why Mohs Surgery Has the Highest Cure Rates
Mohs surgery consistently demonstrates higher cure rates than many other skin cancer treatments. This is due to how the procedure is performed and how cancer cells are identified and removed during surgery.
Complete Margin Examination
Unlike standard skin cancer removal techniques that examine only a small sample of the surgical margins, Mohs surgery allows for complete margin examination. The Mohs surgeon evaluates nearly 100% of the outer and deep edges of the removed tissue under a microscope.
This thorough examination helps identify even small clusters of remaining cancer cells that might otherwise be missed. By confirming that all margins are clear before reconstruction, Mohs surgery reduces the likelihood that cancer cells are left behind.
Layer-by-Layer Precision
Mohs surgery is performed one thin layer at a time. After each layer is removed, it is carefully mapped and examined to determine exactly where cancer cells remain.
This layer-by-layer approach allows the surgeon to:
Target only areas where cancer is present
Preserve as much healthy skin as possible
Stop the procedure as soon as clear margins are achieved
The precision of this process is a key reason Mohs surgery offers strong long-term control of skin cancer while minimizing unnecessary tissue removal.
Factors That Can Affect Success Rates
While Mohs surgery has high overall cure rates, outcomes can vary based on several medical factors. Understanding these variables helps explain why success rates are reported as ranges rather than guarantees.
Tumor Size, Location & Depth
Larger tumors or those that extend deeper into the skin can be more complex to treat. Skin cancers located in areas such as the nose, ears, eyelids, lips, or hands may also have irregular growth patterns.
Tumors in these locations may:
Require additional surgical stages
Extend along nerves or deeper tissue planes
Be more difficult to detect visually
Even in these situations, Mohs surgery remains an effective option because of its precise margin control.
Prior Treatments or Recurrence
Skin cancers that have been treated before and then return are often more challenging. Prior treatments can alter normal tissue and allow cancer cells to grow in less predictable patterns.
Recurrent tumors may:
Spread beyond the original treatment area
Require more extensive removal
Have slightly lower cure rates compared to primary tumors
Mohs surgery is frequently recommended for recurrent skin cancers because it offers the best chance of complete removal.
Surgeon Training & Experience
Mohs surgery is a specialized procedure that requires advanced training in dermatologic surgery, pathology, and reconstruction. Surgeon expertise plays an important role in accurate cancer removal and successful outcomes.
A fellowship-trained Mohs surgeon has:
Specialized education in microscopic tissue analysis
Experience managing complex or high-risk skin cancers
Training in reconstructive techniques following cancer removal
Appropriate training and experience help ensure that Mohs surgery is performed according to established medical standards.
Mohs Surgery vs. Other Skin Cancer Treatments
Several treatment options are available for skin cancer, and the most appropriate choice depends on the type, size, location, and behavior of the tumor. Understanding how Mohs surgery compares to other treatments can help patients better understand why it may be recommended.
Mohs Surgery vs. Standard Excision
Standard surgical excision involves removing the visible tumor along with a margin of surrounding skin. The tissue is then sent to a laboratory, where only a portion of the margins is examined days later.
In contrast, Mohs surgery:
Examines nearly 100% of the surgical margins during the procedure
Confirms complete cancer removal before reconstruction
Preserves more healthy tissue
Has lower recurrence rates for many high-risk tumors
Standard excision is effective for many low-risk skin cancers, while Mohs surgery is often preferred for cancers that require greater precision.
Mohs Surgery vs. Non-Surgical Treatments
Non-surgical treatments for skin cancer may include topical medications, cryotherapy (freezing), photodynamic therapy, or radiation therapy. These approaches may be appropriate for select cases, especially superficial or low-risk cancers.
Compared with non-surgical treatments, Mohs surgery offers:
Direct microscopic confirmation that cancer has been removed
Higher cure rates for many basal and squamous cell carcinomas
Immediate results rather than delayed assessment
Non-surgical treatments do not allow for complete margin examination and may carry a higher risk of recurrence in certain situations. Your dermatologist will recommend the most appropriate option based on your specific diagnosis.
Long-Term Outcomes After Mohs Surgery
Mohs surgery is designed to provide durable, long-term control of skin cancer. While cure rates are high, ongoing skin care and monitoring remain important parts of maintaining long-term health after treatment.
Risk of Recurrence Over Time
Most skin cancers treated with Mohs surgery do not return at the treated site. When recurrence does occur, it is more likely to happen within the first few years after treatment.
The risk of recurrence can depend on:
The type of skin cancer
Whether the tumor was primary or recurrent
Tumor size, depth, and location
Individual health factors
Although Mohs surgery has low recurrence rates, no treatment can completely eliminate the risk, making long-term observation important.
Importance of Follow-Up Care
Regular follow-up visits allow your dermatologist to monitor the surgical site and check for new or recurring skin cancers. Patients who have had one skin cancer are at increased risk of developing others elsewhere on the body.
Follow-up care typically includes:
Routine skin examinations
Monitoring of the healed surgical area
Ongoing sun protection guidance
Consistent follow-up helps support early detection and treatment, which remains the best approach for managing skin cancer over time.
What Success Rates Mean for You as a Patient
Success rates provide helpful context, but they are only one part of the overall treatment picture. Understanding how these statistics apply to individual care can help patients feel informed without creating unrealistic expectations.
Setting Realistic Expectations
Mohs surgery offers high cure rates supported by medical studies, but statistics describe outcomes across large groups of patients. They cannot predict exactly how any one person will heal or respond to treatment.
It is normal for healing to take time, and scars continue to improve over months. While most patients do very well after Mohs surgery, ongoing skin monitoring remains an important part of long-term care.
Individualized Risk Assessment
Each patient’s situation is unique. Factors such as the type of skin cancer, its location, prior treatments, overall health, and immune status all influence treatment planning and outcomes.
Your dermatologist or Mohs surgeon will review these factors and explain how they relate to your diagnosis. This individualized assessment helps guide treatment decisions and follow-up care, ensuring that recommendations are based on your specific medical needs rather than statistics alone.
Frequently Asked Questions About Mohs Surgery Success Rates
Patients often have questions about what Mohs surgery success rates mean and how they relate to individual care. The answers below address common concerns using general medical information and are not a substitute for professional medical advice.
Common Cure-Rate & Outcome Questions
Is Mohs surgery the most effective treatment for skin cancer?
Mohs surgery has some of the highest cure rates for certain basal cell and squamous cell carcinomas, particularly those that are high-risk, recurrent, or located in sensitive areas. Other treatments may be appropriate for lower-risk skin cancers.
Does a high success rate mean the cancer cannot come back?
No treatment can guarantee that skin cancer will never return. While Mohs surgery has low recurrence rates, ongoing follow-up and skin exams remain important.
How long do Mohs surgery cure rates last?
Cure rates are based on long-term studies that follow patients for several years. Most recurrences, if they occur, happen within the first few years after treatment.
Do success rates differ based on where the cancer is located?
Yes. Tumor location, size, depth, and prior treatment history can all influence success rates. Areas with complex anatomy may require more careful management.
Can success rates predict my personal outcome?
Success rates reflect overall trends in large groups of patients. Your individual outcome depends on your specific diagnosis and medical factors, which your Mohs surgeon will discuss with you.
Request a Mohs Consultation